Revolutionizing Healthcare Administration Through Technological Solutions
Revolutionizing Healthcare Administration Through Technological Solutions
A Unified and Automated Approach to Administrative Processes
A Unified and Automated Approach to Administrative Processes

Table of Contents
Chapter 1: The Current State of the U.S. Healthcare Administration Landscape
We stand at the threshold of a new era in healthcare, marked by technological progress, shifts in healthcare practice frameworks, and the impact of a global pandemic on the intricate U.S. healthcare system.
Innovation in healthcare administration is not a distant dream anymore; it's a reality. AI and automation have stepped in and taken over those tasks that once bogged down our healthcare professionals by providing rapid, remotely accessible, and real-time solutions for provider onboarding, payer enrollment, licensing, and many more!
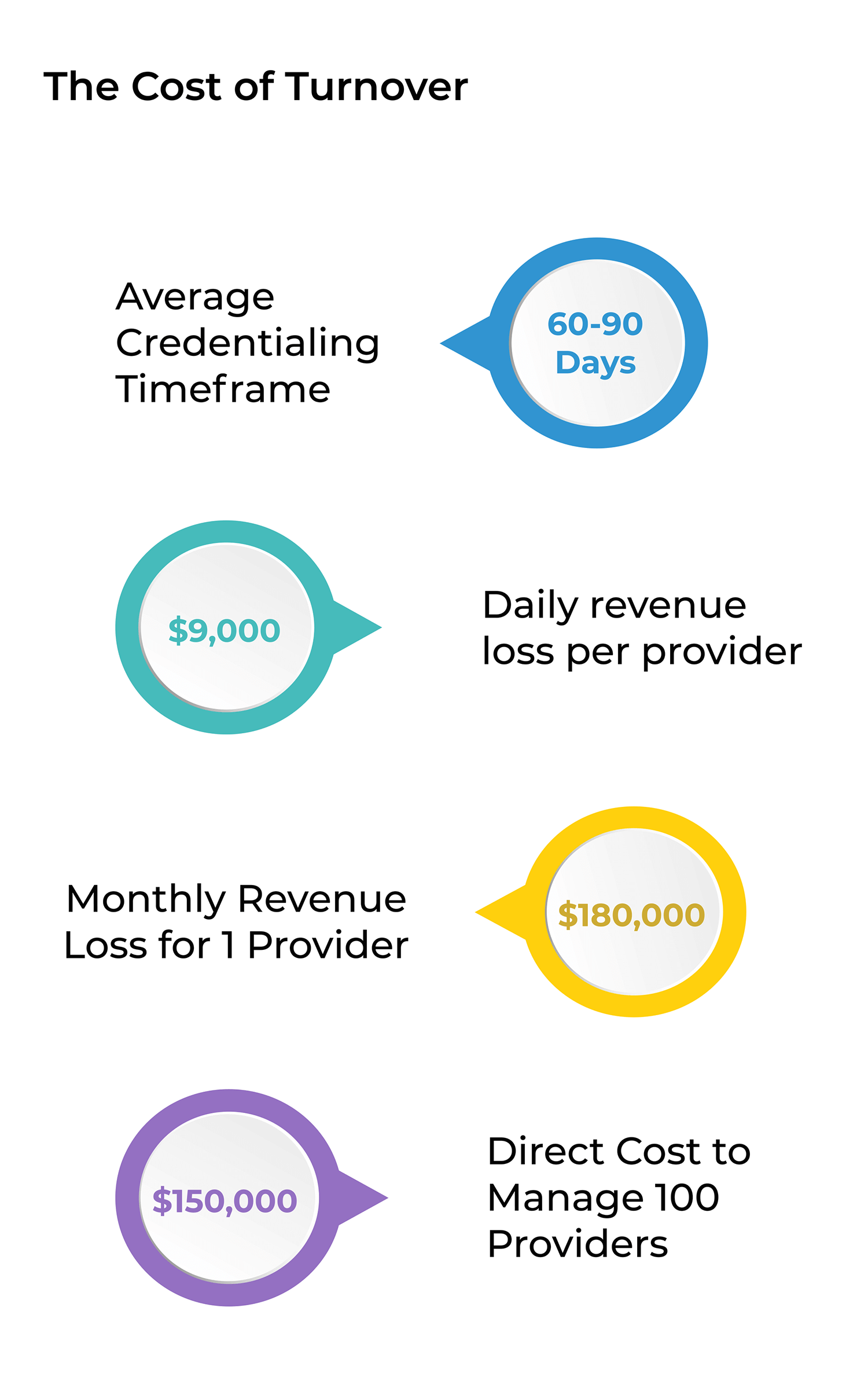
But here's the million-dollar question: Are health systems fully leveraging AI and automation to streamline their cumbersome administrative processes? A recent study found that a whopping 85% of provider credentialing applications have missing critical information which leads to 60-120 days of wasted time. And the financial impact? It’s harsh, costing health systems about $9,000 daily for each provider who is not able to see patients.
And if that's not enough to make you pause – nearly 17% of a physician's precious time is consumed by administrative tasks. Yes, you heard that right. Instead of providing patient care, physicians are navigating paperwork. Beyond just a waste of time, this shift away from patient care is a key player in the rising tide of physician burnout.
So, as we embark on this digital transformation journey in healthcare, the question remains – how can we better integrate these groundbreaking technologies into the American Healthcare System? The aim is clear: enhance administrative efficiency, cut down on those administrative burdens, and most importantly, allow our healthcare professionals to focus on what truly matters: providing exceptional patient care. Let’s dive into this together.

Chapter 2: How Healthcare Professionals Feel About the Current State of Healthcare Administration Landscape
Physician Burnout
Healthcare professionals across the nation are grappling with the growing crisis of burnout. It's a topic that's not just important; it's critical, as it affects the very people we rely on to keep us healthy. Imagine being a physician today; it's not getting any easier. The relentless pressure, the mounting administrative tasks, and the sheer pace at which they're expected to operate are taking a toll.
The conversation around physician burnout isn't new, but it's becoming more urgent. The Medscape Physician Burnout & Depression Report 2022, paints a vivid picture of the situation. 47% of the physicians surveyed admitted experiencing burnout at the workplace.

One physician put it starkly, noting the overwhelming nature of their day-to-day: I barely spend enough time with most patients, just running from one to the next; and then after work, I spend hours documenting, charting, dealing with reports. I feel like an overpaid clerk.
It's not just the mental and emotional toll on doctors; it's the ripple effects this crisis has on patient care. 84% of physicians agreed that their state affects their relationship with patients in some way. A staggering 60% of physicians pointed to the endless bureaucracy as the main culprit for their burnout.
So, what's the way forward? The healthcare industry needs a shift – a move towards systems and processes that recognize the value of physicians' jobs to make their lives easier. This isn't just about improving healthcare; it's about safeguarding it for the future. At the end of the day, a healthy doctor is just as important as a healthy patient.
Turnover
Turnover
High provider turnover rates are a growing problem across the healthcare industry, especially after the pandemic that has intensified the situation. An article by Oracle threw out some staggering numbers related to provider turnover. Hospitals are seeing turnover rates of 19.5%, while at-home care providers and nursing homes are grappling with rates as high as 65% and 94%, respectively, in 2022.
Why are so many physicians leaving? The usual suspects include burnout, over-regulated processes, lack of mentorship, and a buffet of other workplace challenges that have providers hopping from one job to another, sometimes even changing fields entirely. Additionally, providers move between hospitals, health systems, and states throughout their careers. High turnover rates severely impose financial and operational burdens on hospitals and health systems which are already stretched thin to manage rising patient volume.
Healthcare administration teams operate in a high-pressure environment, especially Credentialing and Enrollment staff. These teams drive operational efficiency in health systems but face an uphill battle to keep the gears turning smoothly amidst such high turnover rates.
Chapter 3: Examining the Complexities of Healthcare Administration

Credentialing and Enrollment is a Challenging Journey
Onboarding providers is a complex process filled with tons of moving parts. The goal? To ensure healthcare providers can bill for their services without a hitch. But completing the enrollment process isn't as easy as it sounds. It demands a keen eye, a detail-oriented workflow, and proficiency that many people don’t realize.
Credentialing and enrollment teams verify provider information and process tons of payer enrollments. That’s the key reason why it is essential to have efficient and quick ways to perform credentialing and enrollment so that providers can see patients and start generating revenue sooner.
Healthcare organizations often underestimate the time it takes to complete payer enrollment. Many have yet to grasp just how demanding and information heavy these processes are. And if you don’t get ahead of it, two scenarios could play out:
First, you might find your new provider treating patients before they're officially enrolled with payers. Those services might not be reimbursed, translating to a direct hit to your revenue.
Second, you could end up turning away patients, which also comes with its costs. Once you send them away, the chances of them coming back are slim; they'll likely move on to another provider who's in their network.
So, start early, stay diligent. An automated and efficient onboarding process can benefit everyone involved.
Time-Consuming Workflows
Time-Consuming Workflows
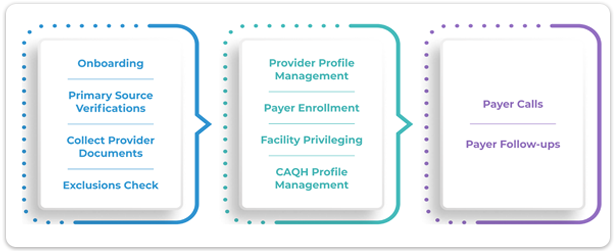
Credentialing and enrollment teams juggle a multitude of tasks to onboard even a single provider. Before a provider joins a hospital or a health system, these meticulous teams dive deep into verifying credentials, double-checking education and training, ensuring all licensing and certification requirements are met, and vetting work history and professional references. Each task demands precision, persistence, and juggling multiple pieces at once. Why? Because every step is crucial in ensuring that providers are not just qualified on paper, but truly ready and able to deliver top-notch care to patients.
The task list to onboard one provider might look overwhelming to the untrained eye, but for these teams, it's all in a day's work. The work of a credentialing and enrollment team is vital to the success of any healthcare organization as they ensure that when we step into a provider's office, we're in capable hands. Let’s take a look at a credentialing and enrollment specialist’s task list to onboard ONE provider.